Pain Procedures in Spine: An Overview
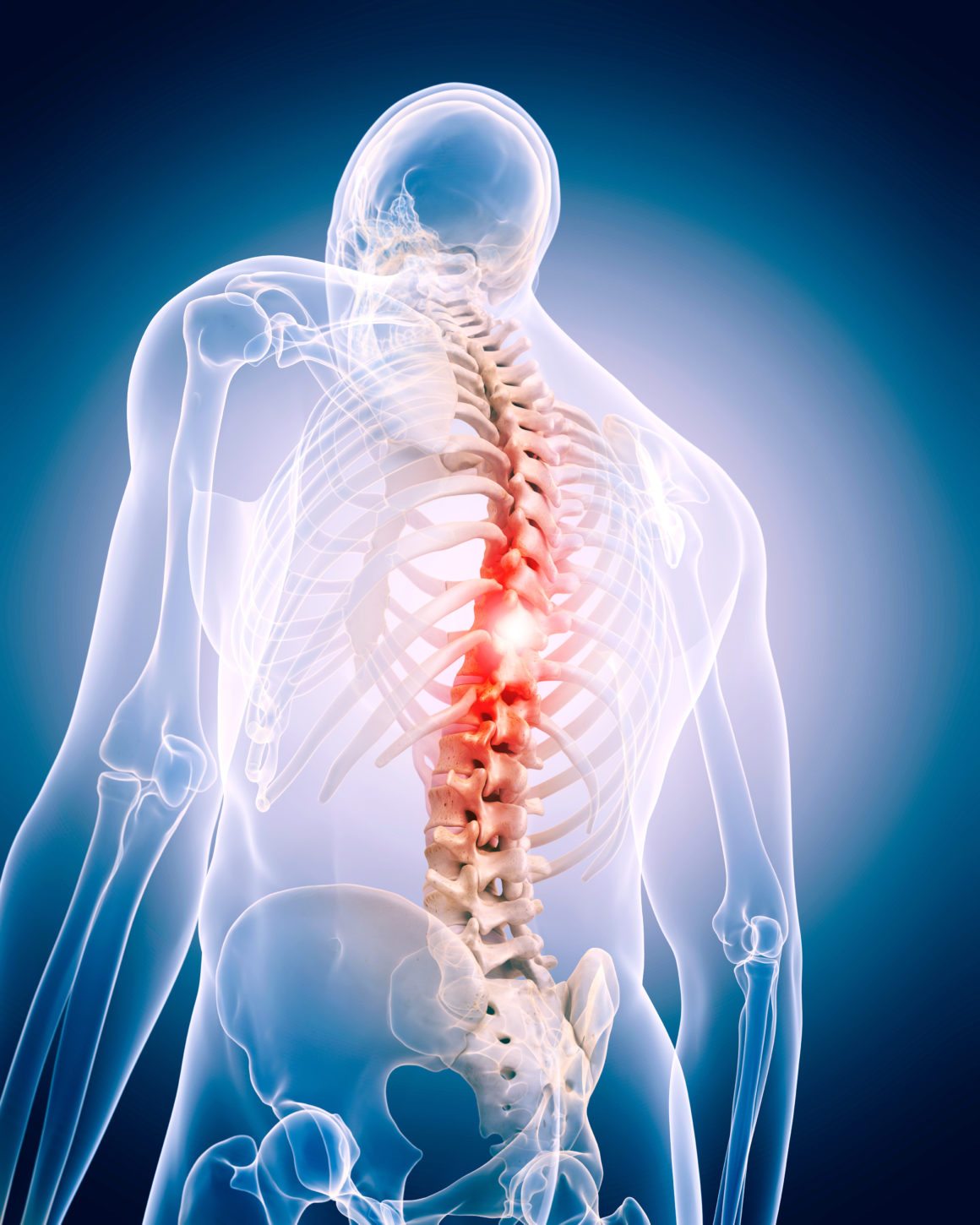
Chronic back pain affects millions worldwide, significantly impacting quality of life. Pain procedures in the spine offer relief when conservative treatments fail. These range from minimally invasive techniques to surgical interventions that alleviate pain and improve function.
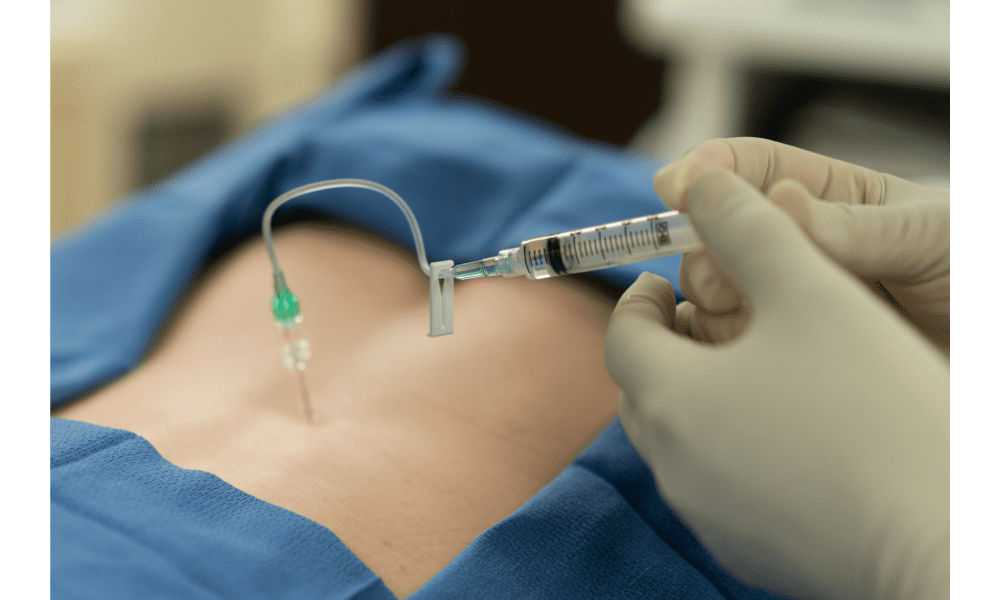
Epidural Steroid Injections (ESI)
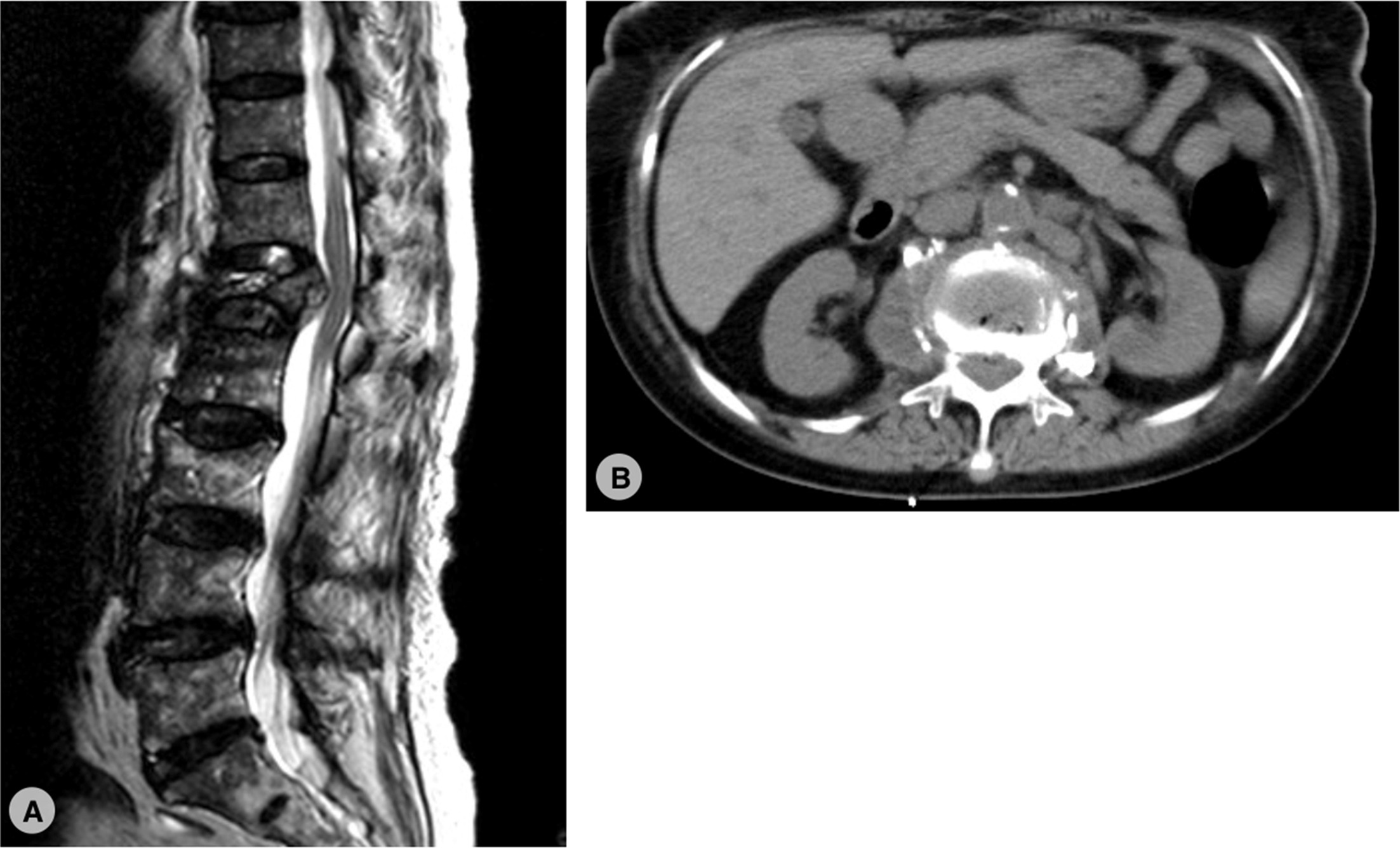
ESI involves injecting corticosteroid medication into the epidural space around the spinal cord and nerve roots to reduce inflammation and alleviate pain caused by conditions such as herniated discs, spinal stenosis, and sciatica. Typically, they provide temporary relief to facilitate rehabilitation efforts.
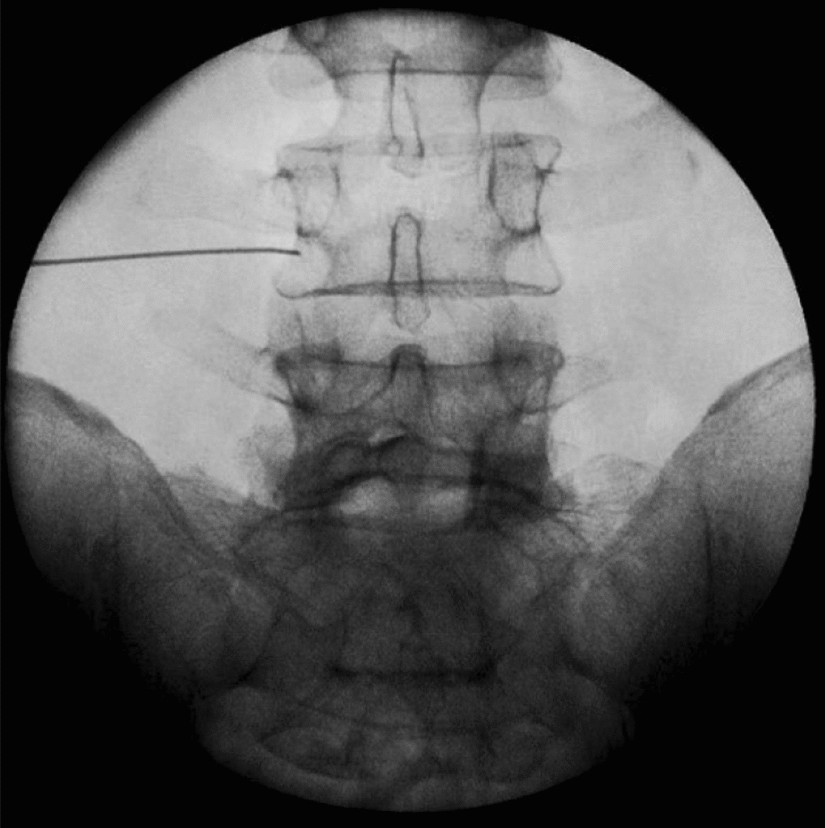
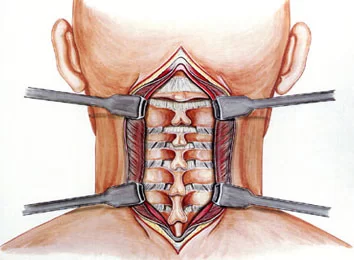
Transforaminal Nerve Root Block
A minimally invasive procedure involving an injection of a local anesthetic and corticosteroid into the spinal nerve's exit point. It treats sciatica, herniated discs, and spinal stenosis, reducing inflammation and improving mobility.
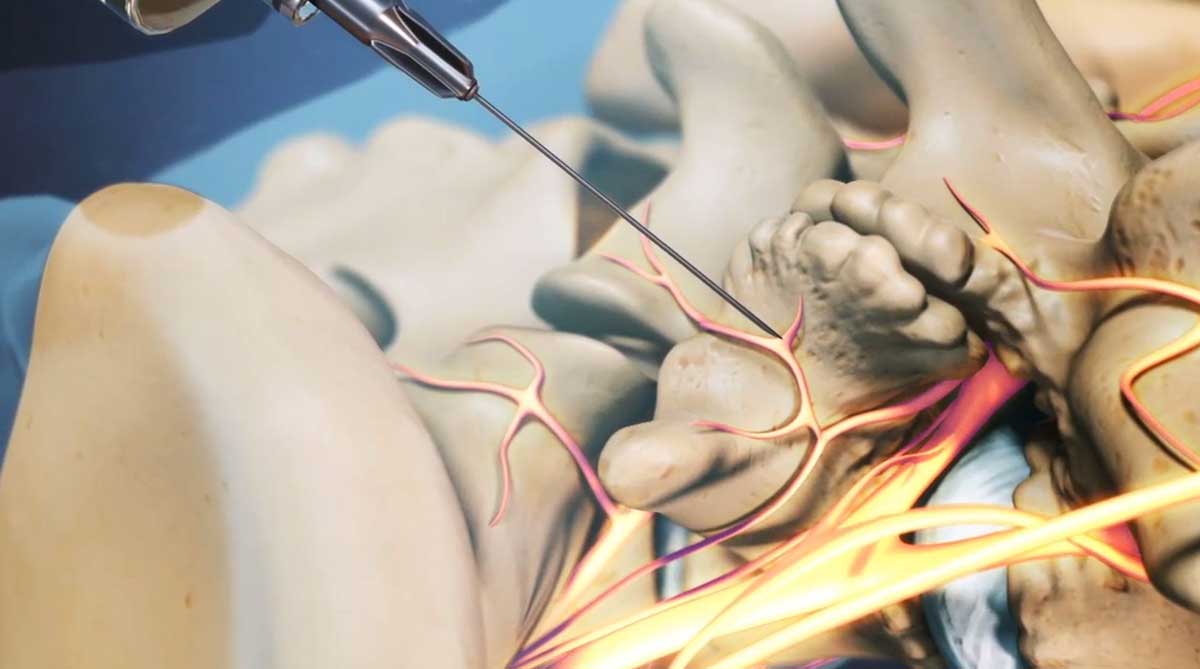
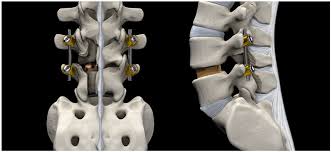
Facet Joint Injections and Medial Branch Blocks
These injections reduce pain in the small facet joints between vertebrae. Facet joint injections deliver anesthetic and steroids directly into the joints, while medial branch blocks target the nerves supplying these joints.
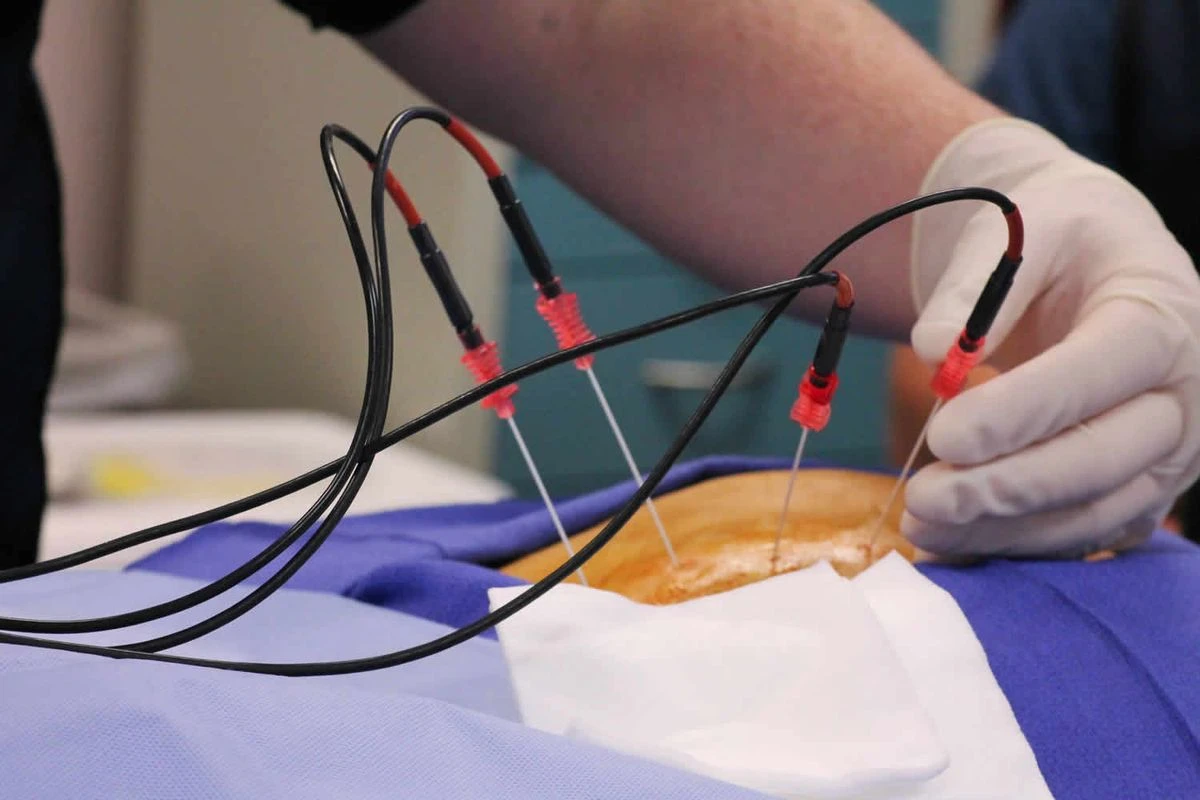
Radiofrequency Ablation (RFA)
This technique ablates nerve fibers responsible for carrying pain signals, offering long-term relief for up to a year. It is often used following successful medial branch blocks to treat chronic pain from the facet joints.

Spinal Cord Stimulation (SCS)
SCS involves implanting a device that sends electrical impulses to the spinal cord, blocking pain signals. It is typically used for conditions like failed back surgery syndrome and neuropathic pain. A trial period with an external stimulator precedes permanent implantation.
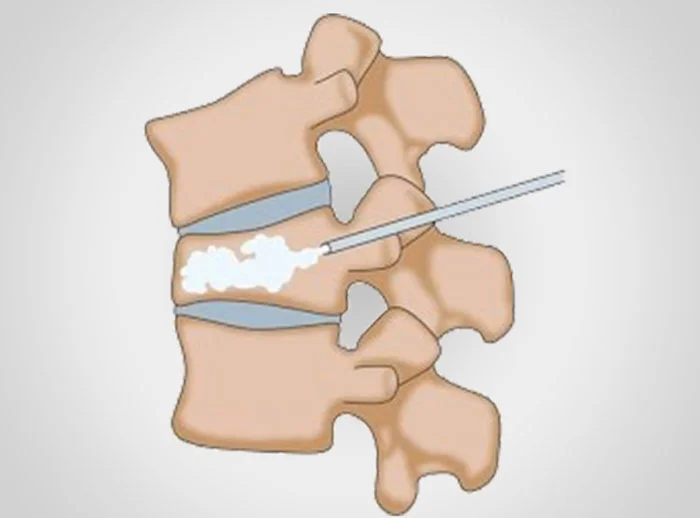
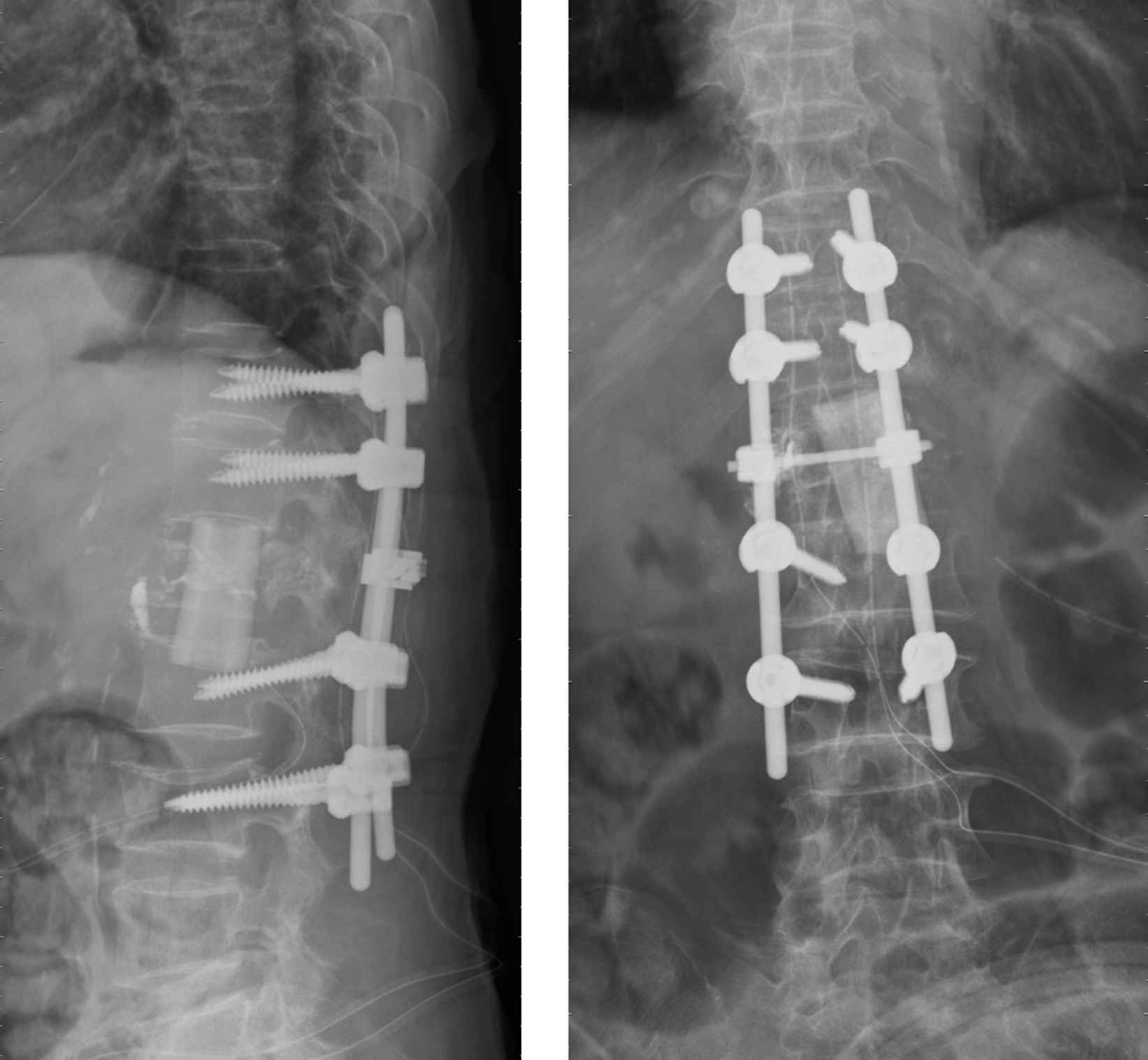
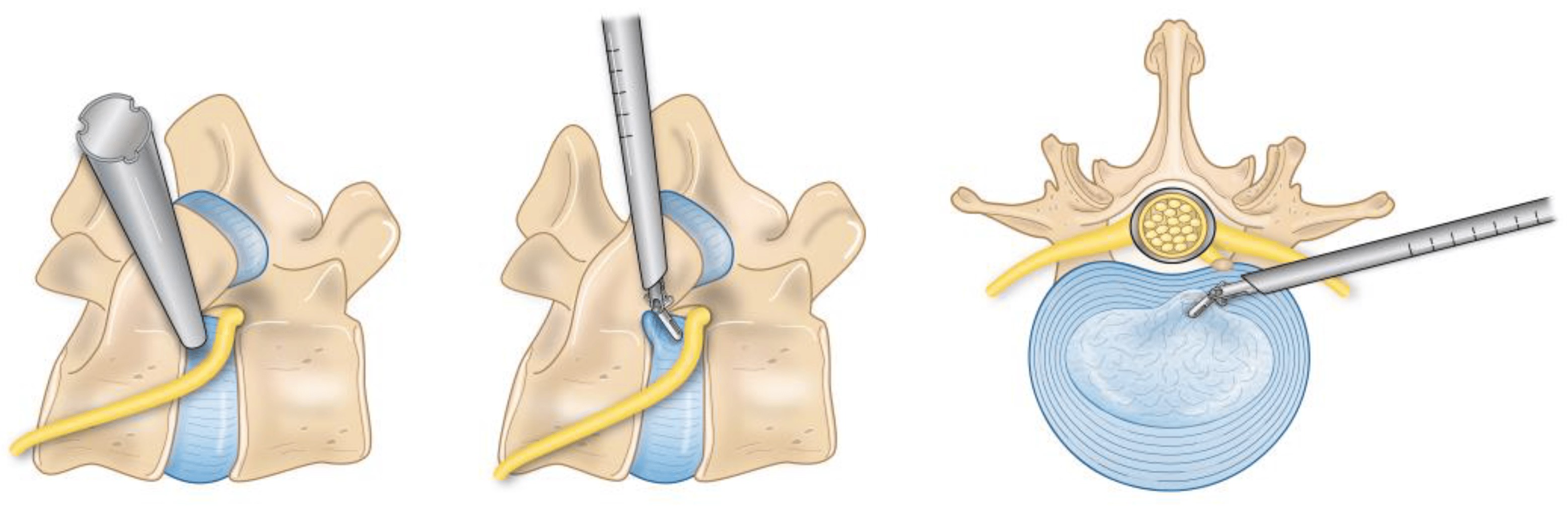
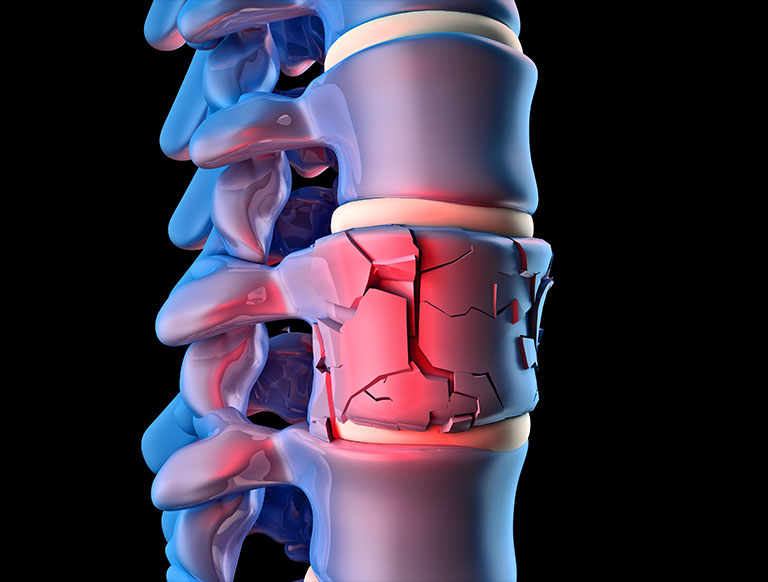
Vertebroplasty and Kyphoplasty
These procedures treat spinal compression fractures, often due to osteoporosis. Vertebroplasty injects cement into fractured vertebrae, while kyphoplasty creates space using a balloon before cement injection to restore vertebral height and stability.
Considerations and Risks
While spine pain procedures offer significant relief, potential complications include infection, bleeding, nerve damage, and allergic reactions to medications. Proper patient selection and thorough diagnostic evaluation are crucial to minimize risks and ensure successful outcomes.
Conclusion
Pain procedures in the spine are essential in modern pain management. When appropriately selected, these interventions can provide significant pain relief, improve function, and enhance quality of life. They should be part of a comprehensive treatment plan, including physical therapy and lifestyle modifications.