Sciatica/ Radiculopathy: An Overview
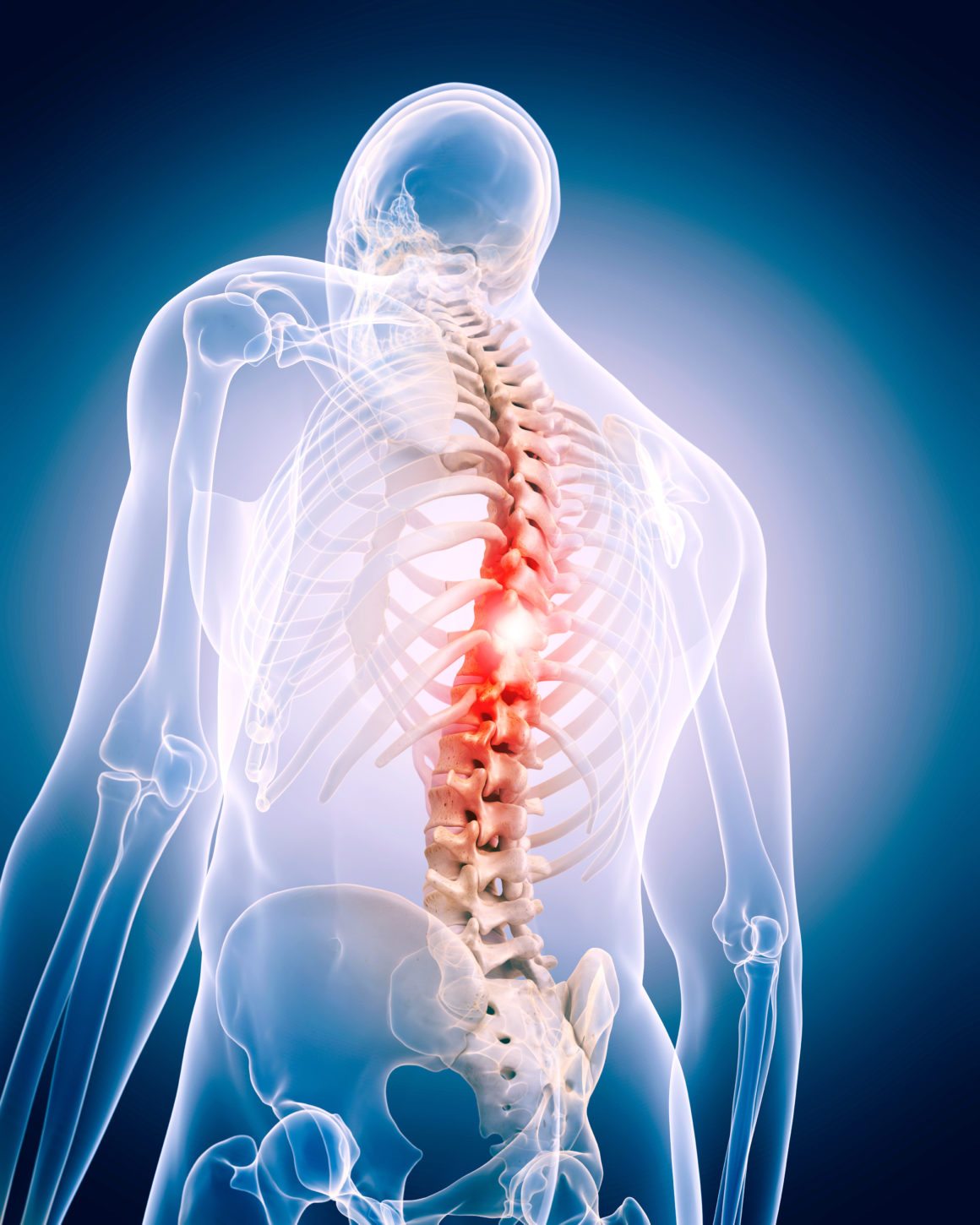
Sciatica is a common condition characterized by pain that radiates along the path of the sciatic nerve, which extends from the lower back through the hips and buttocks and down each leg. Typically, sciatica affects only one side of the body and is often associated with tingling, numbness, or muscle weakness in the affected leg. Understanding the causes, symptoms, and available treatments for sciatica is essential for managing this often-debilitating condition.
Causes of Sciatica
Sciatica occurs when the sciatic nerve becomes pinched or compressed. The most common causes include:
- Herniated Disc: A herniated or slipped disc occurs when the soft inner gel of a spinal disc protrudes through its outer layer, pressing on the nearby sciatic nerve. This is the most frequent cause of sciatica.
- Trauma or Injury: Accidents or injuries that affect the lower spine can also lead to sciatic nerve compression.
Symptoms of Sciatica
The primary symptom of sciatica is pain that radiates from the lower back to the buttock and down the back of the leg. Other symptoms may include:
- Sharp, Burning Pain: The pain can range from a mild ache to a sharp, burning sensation that can be excruciating in some cases.
- Numbness or Tingling: Patients may experience numbness or a tingling sensation in the affected leg or foot.
- Weakness: Muscle weakness in the leg or foot, making it difficult to move or control the affected limb.
- Worsening Pain with Movement: Symptoms often worsen with prolonged sitting, standing, or sudden movements.
Diagnosis of Sciatica
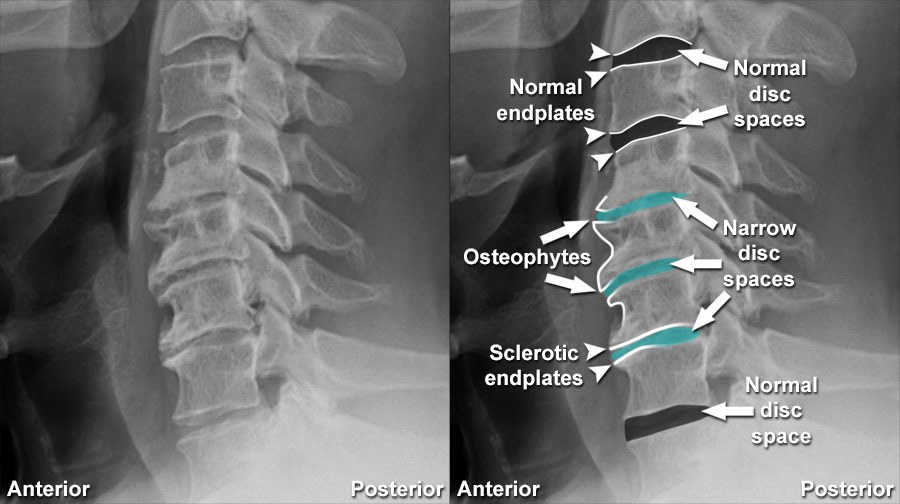
Diagnosing sciatica involves a combination of a physical examination and imaging tests. Doctors may perform tests to assess muscle strength and reflexes. Imaging tests, such as X-rays, MRI, or CT scans, can help identify the underlying cause of nerve compression, such as a herniated disc or spinal stenosis.
Treatment Options for Sciatica
The treatment of sciatica focuses on relieving pain and addressing the underlying cause of nerve compression. Treatment options include:
- Medication: Over-the-counter pain relievers, anti-inflammatory drugs, and muscle relaxants can help reduce pain and inflammation.
- Physical Therapy: A physical therapist can design a customized exercise program to improve flexibility, strength, and posture, which can help alleviate pressure on the sciatic nerve.
- Corticosteroid Injections: In some cases, corticosteroid injections near the affected nerve root can reduce inflammation and provide temporary pain relief.
- Alternative Therapies: Some patients find relief through alternative therapies such as acupuncture, chiropractic adjustments, or massage therapy.
- Surgery: Surgery may be considered when conservative treatments fail to relieve symptoms or if the patient experiences severe pain, weakness, or loss of bowel or bladder control. Common surgical procedures include discectomy or laminectomy to remove the source of nerve compression.
- Endoscopic Discectomy / Decompression: This is the current gold standard treatment for sciatica and disc prolapse, offering minimally invasive relief for nerve compression.
Prevention of Sciatica
Preventing sciatica involves maintaining a healthy lifestyle and minimizing strain on the lower back. Key preventive measures include:
- Regular Exercise: Engaging in regular physical activity, including exercises that strengthen the core muscles and improve flexibility, can help support the spine and reduce the risk of sciatica.
- Proper Lifting Techniques: Using proper lifting techniques and avoiding heavy lifting can prevent strain on the lower back.
- Good Posture: Maintaining good posture while sitting, standing, and sleeping can help reduce stress on the spine and prevent nerve compression.
- Weight Management: Maintaining a healthy weight reduces pressure on the spine and decreases the risk of disc herniation and other back problems.
Conclusion
Sciatica is a common and often painful condition that affects millions of people worldwide. Understanding its causes, symptoms, and treatment options is essential for effectively managing the condition and improving the quality of life for those affected. While sciatica can be debilitating, a combination of medical treatment, lifestyle modifications, and preventive measures can help alleviate pain and prevent recurrence. By taking proactive steps to maintain spinal health and addressing symptoms early, individuals can reduce the impact of sciatica on their daily lives.
Endoscopic Discectomy / Decompression is the current gold standard treatment for Sciatica and disc prolapse.
Compressive Myelopathy: Understanding, Causes, and Management
Compressive myelopathy is a medical condition characterized by the compression of the spinal cord, resulting in neurological deficits. This compression can be caused by a variety of factors and is considered a serious medical condition that requires prompt diagnosis and treatment. Understanding the causes, symptoms, diagnostic approaches, and treatment options for compressive myelopathy is crucial for effective management and improving patient outcomes.
Causes and Risk Factors
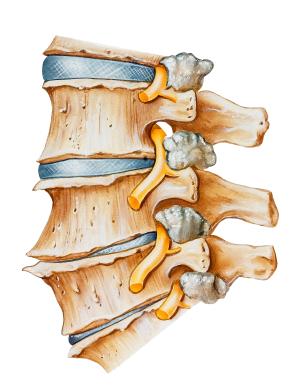
Compressive myelopathy can be caused by a range of factors, including degenerative, traumatic, neoplastic, infectious, and congenital conditions. One of the most common causes is degenerative disc disease, which leads to the formation of herniated discs or osteophytes (bone spurs) that impinge on the spinal cord. Traumatic injuries, such as those sustained in car accidents or falls, can also result in spinal fractures or dislocations that compress the cord.
Neoplasms, or tumors, whether primary or metastatic, may grow within or adjacent to the spinal canal and exert pressure on the spinal cord. Additionally, infections such as spinal epidural abscesses or tuberculosis can lead to compressive lesions. Congenital abnormalities, like Arnold-Chiari malformation or tethered cord syndrome, may also result in spinal cord compression.
Risk factors for compressive myelopathy include age, which is associated with degenerative changes, a history of spinal trauma, cancer with potential metastasis to the spine, and certain congenital conditions.
Symptoms
The symptoms of compressive myelopathy vary depending on the location and extent of spinal cord compression. Common symptoms include:
- Pain: Localized pain in the neck or back is often the first symptom, which may radiate to the arms or legs.
- Numbness and Tingling: Patients frequently experience sensory deficits, including numbness or tingling in the extremities.
- Weakness: Muscle weakness can occur, affecting the arms, legs, or both, depending on the level of compression.
- Coordination and Gait Disturbances: Difficulty walking, balance problems, and coordination issues are common as the condition progresses.
- Bladder and Bowel Dysfunction: In severe cases, patients may experience incontinence or difficulty with bladder and bowel control.
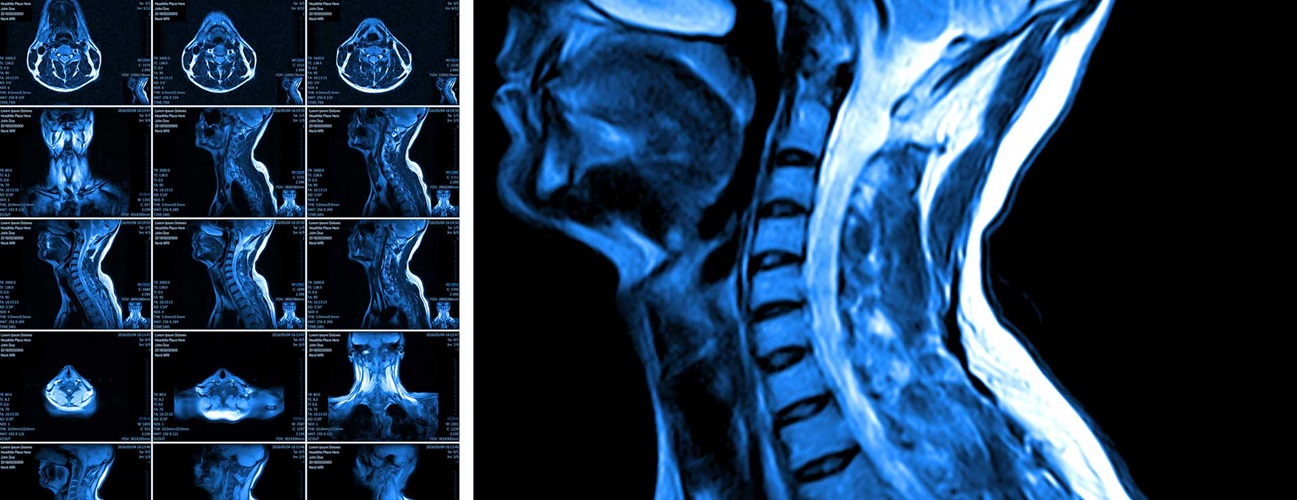
Diagnosis
Diagnosing compressive myelopathy involves a combination of clinical evaluation and imaging studies. A thorough neurological examination can identify deficits and help localize the level of compression. Imaging studies, particularly magnetic resonance imaging (MRI), are crucial in visualizing the spinal cord, identifying the source of compression, and assessing its severity. Computed tomography (CT) scans and X-rays may also be used to evaluate bony structures and traumatic injuries.
Treatment
The treatment of compressive myelopathy depends on the underlying cause and the severity of symptoms. In cases of acute spinal cord compression, surgical intervention is often required to relieve pressure and prevent further neurological damage. Surgical options may include decompression laminectomy, discectomy, or tumor resection.
In less severe cases or when surgery is not immediately indicated, conservative management may be employed. This can involve physical therapy, pain management, and medications such as corticosteroids to reduce inflammation. In cases of infectious myelopathy, antibiotics or antifungal medications are necessary to address the underlying infection.
Conclusion
Compressive myelopathy is a serious medical condition that requires prompt recognition and treatment to prevent permanent neurological damage. By understanding the causes, symptoms, and treatment options, healthcare providers can improve patient outcomes and quality of life. Advances in imaging technology and surgical techniques continue to enhance the ability to diagnose and treat this challenging condition effectively.
Degenerative Spine
The term "degenerative spine" refers to the natural wear and tear of the spine's structures—such as discs, joints, and bones—over time. This process is often associated with aging but can also result from injuries, genetic predisposition, or lifestyle factors. The degeneration can lead to conditions like herniated discs, osteoarthritis, and spinal stenosis, causing pain, reduced mobility, and nerve-related symptoms.
Causes
Degenerative spine conditions arise primarily from the natural aging process, during which spinal discs lose hydration and elasticity, leading to wear and tear. Factors like genetics, obesity, smoking, and poor posture can accelerate degeneration. Repetitive stress from physical labor, injuries, or trauma also contributes to spinal damage. Additionally, conditions like osteoarthritis and herniated discs can exacerbate the deterioration of the spine's structure over time.
Symptoms
- Pain:Chronic back or neck pain, especially in the lower back (lumbar) or neck (cervical) regions.
- Stiffness:Difficulty bending, twisting, or straightening the back.
- Nerve-Related Issues: Numbness or tingling in the arms, legs, or other extremities, Weakness in the muscles, Shooting pain, such as sciatica, radiating down the leg.
- Reduced Mobility:Difficulty performing daily tasks,Loss of flexibility in the spine.
- Deformity:Visible changes in posture, such as a hunched back.
Treatment
Treatment for a degenerative spine focuses on symptom management and improving quality of life. Non-surgical options include pain relief medications, physical therapy for strengthening and flexibility, and lifestyle changes like weight management and ergonomic adjustments. For severe cases, surgical interventions such as spinal fusion, laminectomy, or artificial disc replacement may be necessary to restore function and alleviate nerve compression. Alternative therapies like acupuncture, chiropractic care, and yoga can also provide symptom relief for some individuals.
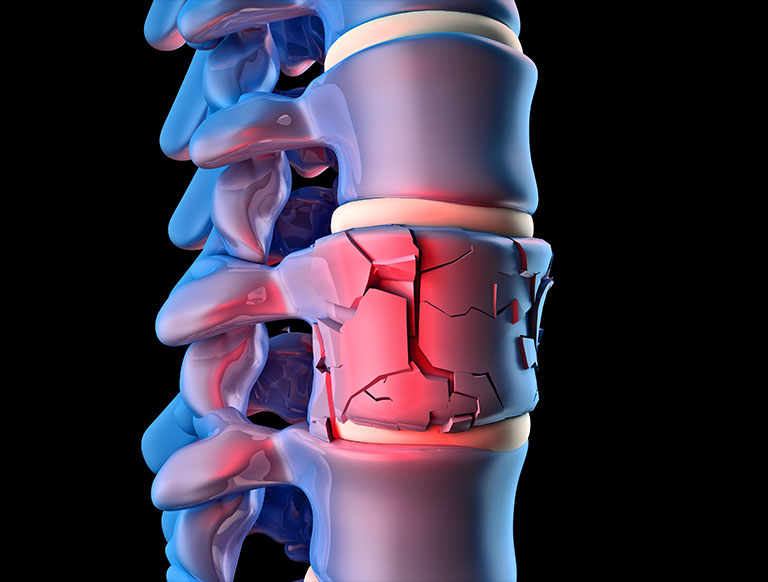
Osteoporotic Spine Fractures: Causes, Impact, and Treatment Strategies
Osteoporotic spine fractures are a prevalent health issue, particularly among the elderly, characterized by fractures in the vertebrae due to weakened bone strength from osteoporosis. These fractures are a significant source of pain, disability, and reduced quality of life, making their prevention and treatment critical for maintaining the health and well-being of affected individuals.
Understanding Osteoporosis
Osteoporosis is a systemic skeletal disease characterized by low bone mass and microarchitectural deterioration of bone tissue, leading to increased bone fragility and susceptibility to fractures. It is often referred to as a "silent disease" because it progresses without symptoms until a fracture occurs. The spine, hip, and wrist are the most common sites of osteoporotic fractures.
Causes of Osteoporotic Spine Fractures
Osteoporotic spine fractures, also known as vertebral compression fractures (VCFs), occur when the vertebrae become so weak that even minor stresses, such as bending, lifting, or coughing, can cause them to collapse. The primary cause of these fractures is the loss of bone density associated with osteoporosis. Several factors contribute to osteoporosis, including:
- Age: Bone density decreases naturally with age, making older adults particularly susceptible.
- Gender: Women are at higher risk due to lower peak bone mass and the rapid bone loss that occurs after menopause.
- Genetics: A family history of osteoporosis or fractures increases risk.
- Lifestyle Factors: Poor diet, smoking, excessive alcohol consumption, and sedentary lifestyle can contribute to bone loss.
- Medications and Medical Conditions: Certain medications (e.g., corticosteroids) and medical conditions (e.g., rheumatoid arthritis) can accelerate bone loss.
Symptoms and Impact
Osteoporotic spine fractures can lead to a range of symptoms and complications. Acute fractures often cause sudden, severe back pain that may be accompanied by limited mobility and tenderness over the affected vertebra. In some cases, pain may radiate to the abdomen or flank. Chronic fractures can result in spinal deformities, such as kyphosis (a forward curvature of the spine), which can lead to a stooped posture.
The impact of vertebral fractures extends beyond physical symptoms. They can significantly affect quality of life, leading to decreased mobility, loss of independence, and increased risk of further fractures. Additionally, vertebral fractures are associated with an increased risk of mortality due to complications such as deep vein thrombosis and pulmonary embolism.
Diagnosis and Treatment
Diagnosis of osteoporotic spine fractures typically involves a combination of clinical evaluation and imaging studies. X-rays are commonly used to identify vertebral compression fractures, while bone density tests, such as dual-energy X-ray absorptiometry (DEXA), are used to assess the severity of osteoporosis.
Treatment of osteoporotic spine fractures focuses on relieving pain, stabilizing the spine, and preventing future fractures. Non-surgical treatments include:
- Pain Management: Medications such as analgesics and anti-inflammatory drugs can help manage pain.
- Bracing: Spinal braces may provide support and limit movement to promote healing.
- Physical Therapy: Exercises to improve strength, flexibility, and posture can aid recovery and prevent further injury.
In cases where conservative treatment is insufficient, minimally invasive surgical procedures such as vertebroplasty or kyphoplasty may be considered. These procedures involve injecting bone cement into the fractured vertebra to stabilize it and alleviate pain.
Preventive strategies, such as calcium and vitamin D supplementation, weight-bearing exercises, and medications like bisphosphonates, are crucial for managing osteoporosis and reducing the risk of future fractures.
Conclusion
Osteoporotic spine fractures pose a significant health challenge, particularly among older adults. Understanding the causes, impact, and treatment options is essential for improving patient outcomes and enhancing quality of life. With advances in medical care and an emphasis on preventive strategies, it is possible to mitigate the effects of osteoporosis and reduce the burden of vertebral fractures on individuals and healthcare systems.
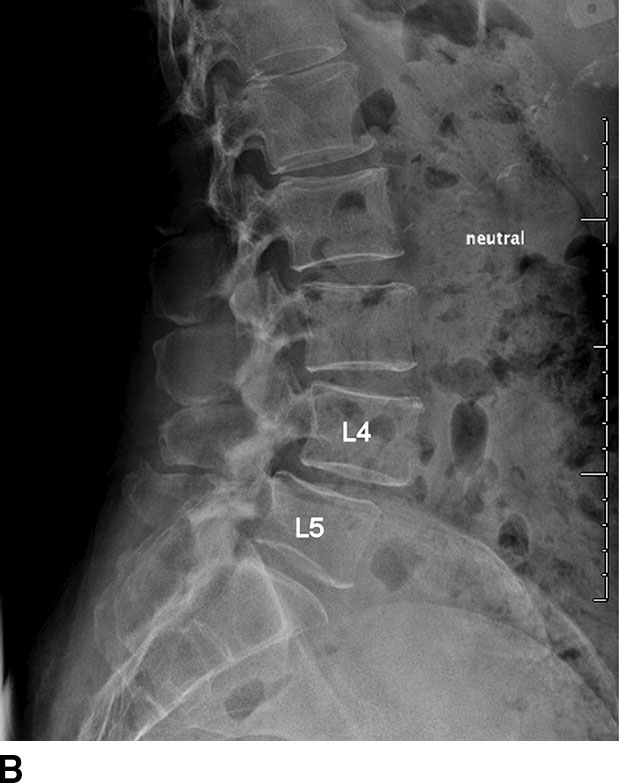
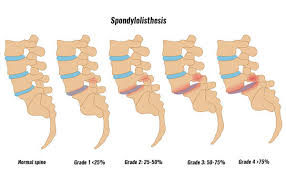
Spondylolisthesis
Spondylolisthesis is a condition in which one vertebra in the spine slips forward or backward over the one below it. It commonly affects the lower back, especially the lumbar spine, and can cause a range of symptoms that impact mobility and quality of life. Understanding the anatomy, pathology, symptoms, and treatment options for spondylolisthesis can help patients better manage the condition.
Anatomy:
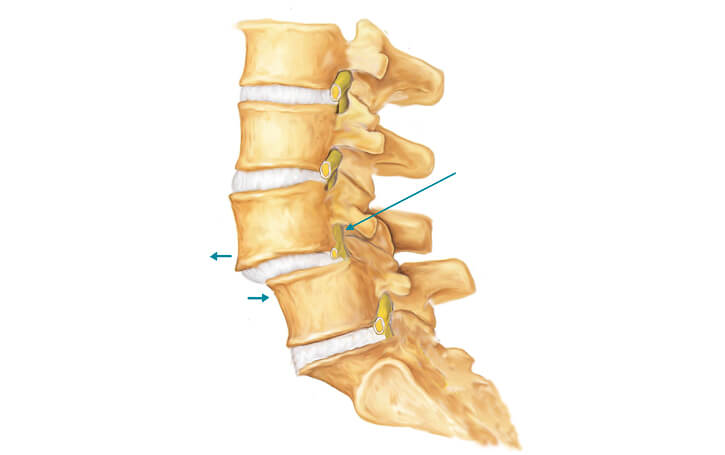
The spine consists of 33 vertebrae stacked on top of each other, separated by intervertebral discs that act as cushions. Ligaments and muscles provide stability and movement. In spondylolisthesis, the misalignment occurs when a vertebra slips out of place, often due to a defect in the bone (spondylolysis) or degeneration of the disc and joints that hold the vertebrae together.
Pathology:
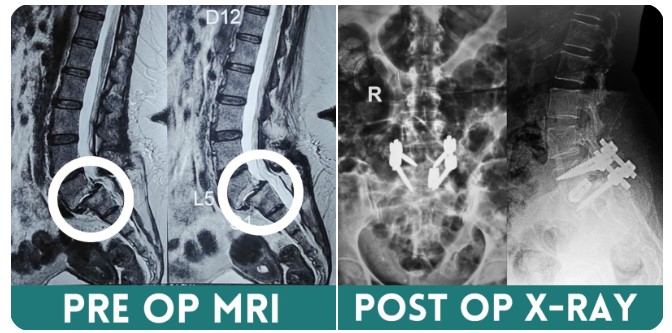
Spondylolisthesis can result from congenital factors, trauma, degenerative changes, or repetitive stress. As the vertebra shifts, it may compress nerves in the spinal canal, leading to discomfort or pain. This condition is graded on the severity of the slip, ranging from mild to severe.
Symptoms:
Common symptoms include lower back pain, stiffness, and tenderness. In more severe cases, patients may experience leg pain, numbness, weakness, or difficulty walking due to nerve compression. These symptoms can worsen with activity or prolonged standing.
Treatment:
Treatment typically begins with conservative measures such as rest, physical therapy, and pain management. If symptoms persist or worsen, surgical options like spinal fusion may be considered to stabilize the spine. Surgery is generally reserved for severe cases where conservative treatments fail to provide relief.
Early diagnosis and appropriate treatment are key to managing spondylolisthesis and improving quality of life
Traumatic Spine Surgery: Challenges and Advances
Traumatic spine surgery is a specialized field focused on treating injuries to the spinal column and spinal cord resulting from trauma. These injuries can arise from various causes, including vehicular accidents, falls, sports injuries, or acts of violence. The primary goal of traumatic spine surgery is to stabilize the spine, relieve pressure on the spinal cord and nerves, and restore as much function as possible. Understanding the complexities, advancements, and challenges involved in these procedures provides valuable insights into spinal trauma care.
Nature and Impact of Spinal Trauma
Spinal trauma can lead to a range of injuries, from fractures and dislocations of the vertebrae to severe spinal cord injuries (SCI) that may result in partial or complete paralysis. Beyond the physical damage, these injuries often affect the psychological and social aspects of a patient's life. Immediate and effective treatment is crucial to minimize long-term disabilities and improve the overall quality of life for affected individuals.
Indications for Traumatic Spine Surgery
Surgical intervention is often required in cases where the spine is unstable, there is significant compression of neural elements, or when conservative treatment fails to provide adequate results. Common indications for traumatic spine surgery include:
- Spinal Fractures: Fractures that compromise the stability of the spine or impinge on the spinal cord may require surgical stabilization using rods, screws, or plates.
- Dislocations: Misaligned vertebrae due to dislocation may need surgical realignment and stabilization to prevent further damage.
- Spinal Cord Compression: Surgery is often necessary to relieve pressure on the spinal cord caused by bone fragments, herniated discs, or hematomas.
Challenges in Traumatic Spine Surgery
Traumatic spine surgery is inherently complex and presents several challenges, including:
- Timing: Determining the optimal timing for surgery can be difficult, as early intervention may reduce secondary damage but increases the risk of complications.
- Complex Anatomy: The intricate anatomy of the spine, coupled with the presence of critical neural elements, requires precise surgical technique and expertise.
- Variability of Injuries: Each spinal injury is unique, necessitating a personalized approach to surgical planning and execution.
- Risk of Complications: Surgical risks include infection, bleeding, nerve damage, and the potential for further destabilization of the spine.
Advances in Surgical Techniques
Recent advancements in technology and surgical techniques have significantly improved outcomes in traumatic spine surgeries:
- Minimally Invasive Techniques: These approaches reduce tissue disruption, lower infection risks, and promote quicker recovery.
- Advanced Imaging and Navigation: Real-time imaging and computer-assisted navigation enhance surgical precision and accuracy, reducing the risk of complications.
- Robotic-Assisted Surgery: Robotics offers greater precision in implant placement, which is crucial in complex spinal reconstructions.
- Neuroprotective Strategies: Techniques to minimize spinal cord injury during surgery, such as hypothermia and pharmacological interventions, are being explored to improve neurological outcomes.
Rehabilitation and Recovery
Recovery from traumatic spine surgery requires a multidisciplinary approach, including physical therapy, occupational therapy, and psychological support. Rehabilitation focuses on maximizing functional independence, improving mobility, and managing pain. The extent of recovery depends on the severity of the initial injury, the success of the surgical intervention, and the individual’s overall health and motivation.
Conclusion
Traumatic spine surgery plays a critical role in managing spinal injuries resulting from trauma. Despite the challenges, advances in surgical techniques and technologies have greatly enhanced the ability to stabilize the spine, relieve neural compression, and improve patient outcomes. A comprehensive approach involving timely surgical intervention, rehabilitation, and ongoing support is essential for optimizing recovery and enhancing the quality of life for individuals affected by spinal trauma. Continued research and innovation in the field offer hope and improved prognoses for those suffering from these life-altering injuries.